I am just entering my third week of recovery from an open myomectomy and this has hands down been the most painful and difficult challenge I have ever faced in my entire life.
I am noticing my body changes after myomectomy, minding a nutritious fibroids recovery diet and overall, there has been progress. I have decided to share what my recovery week by week has looked like so far and would continue sharing over the next weeks.
*Warning, some people may not be comfortable with some of the images in this post. Proceed with this in mind*
1) Body changes: Within the first week of my myomectomy, I dropped about 15 pounds. 15 POUNDS! That is a very significant amount of weight to lose within days.
I attribute most of the weight loss to the the fibroids (unfortunately my doctor did not take any photos nor provide their weight) as they were very voluminous. Some of the weight is probably fluid and blood loss (2 litres of blood lost during surgery) in addition to the first week’s decreased calorie consumption.
Before surgery, I was told I had one very large fibroid (13cm) and then a smaller one, about 9cm, and then 3 or 4 smaller ones (5cm or below).
During my myomectomy, 2 more larger fibroids were discovered. One was about 13cm and the other was 11cm. None of my ultrasounds nor MRI scans had picked them up. I remember mentioning before surgery that I had a feeling there may be more and I would not be surprised if they discovered more fibroids during my surgery. I ended up being right about that.
My surgery ended up taking about 4 hours, rather than the 1.5 hours they had estimated. I woke up in a lot of pain and with a swollen abdomen (which is normal).
 Not only was my abdomen swollen and stitched tight but my face was also swollen, probably from all the fluids that were being injected into my body. The facial swelling went down within the first week but the abdomen is still pretty swollen and would take 6 weeks or more to go back to its original size.
Not only was my abdomen swollen and stitched tight but my face was also swollen, probably from all the fluids that were being injected into my body. The facial swelling went down within the first week but the abdomen is still pretty swollen and would take 6 weeks or more to go back to its original size.
This is because my uterus needs time to shrink after being stretched out by fibroids for so long. It takes about 6 weeks for the uterus to heal after a myomectomy.
I don’t even know what my ‘normal’ stomach would look like at the end of this.
Everyone says I have noticeably lost weight (not just in the abdomen) and I’m not sure I can explain that especially now that my appetite is fully back.
Now let’s talk about my incision. I ended up having to need a vertical incision instead of the more common horizontal C-section cut. My belly also had to be stapled shut post-surgery (see graphic photo below). I noticed an itching sensation around the incision around day 4 and was told this was good as it meant the incision was healing.
I noticed an itching sensation around the incision around day 4 and was told this was good as it meant the incision was healing.
After a week, the staples were taken off but a part of the incision remained open and so surgical tape was placed on top of it. I was told to take it off after a week but unfortunately, even after the second week, part of the incision was still open.
Thankfully it is not infected but it just means my incision would probably take more time to close up, dry and heal. It’s been scabbing more this week, which is good and I just have to keep fighting the urge to keep touching it and let my body do its thing.
I’m being mindful not to let it get moist (which would harbour bacteria) and to keep it nice and aired out. I also had to dial it back a little with my already limited physical activity just because I do not want to put any unnecessary pressure on the wound.
Coughing and sneezing are the scariest because it almost feels like the wound might rip open from the pressure. I ensure to always press a pillow or both my hands on my abdomen whenever I need to cough or sneeze.
If you recall, I had prepared for my myomectomy recovery as seen here. These items have come in handy!
2) Diet: Even before my myomectomy, I had already planned on what my nutrition would look like post-surgery. I wanted to limit fatty foods and stock up on nutritious foods and snacks.
The day of my surgery, all I could stomach was a few spoonfuls of mashed potatoes and water. I had no appetite whatsoever and only consumed the mash potatoes because I was on very strong pain meds (morphine) and did not want to be taking those on a completely empty stomach.
Remember that you are required to fast for 12 hours prior to surgery and no water consumption neither. So I had not eaten nor drank in 24 hours by the time I was settled down into my hospital room and bed.
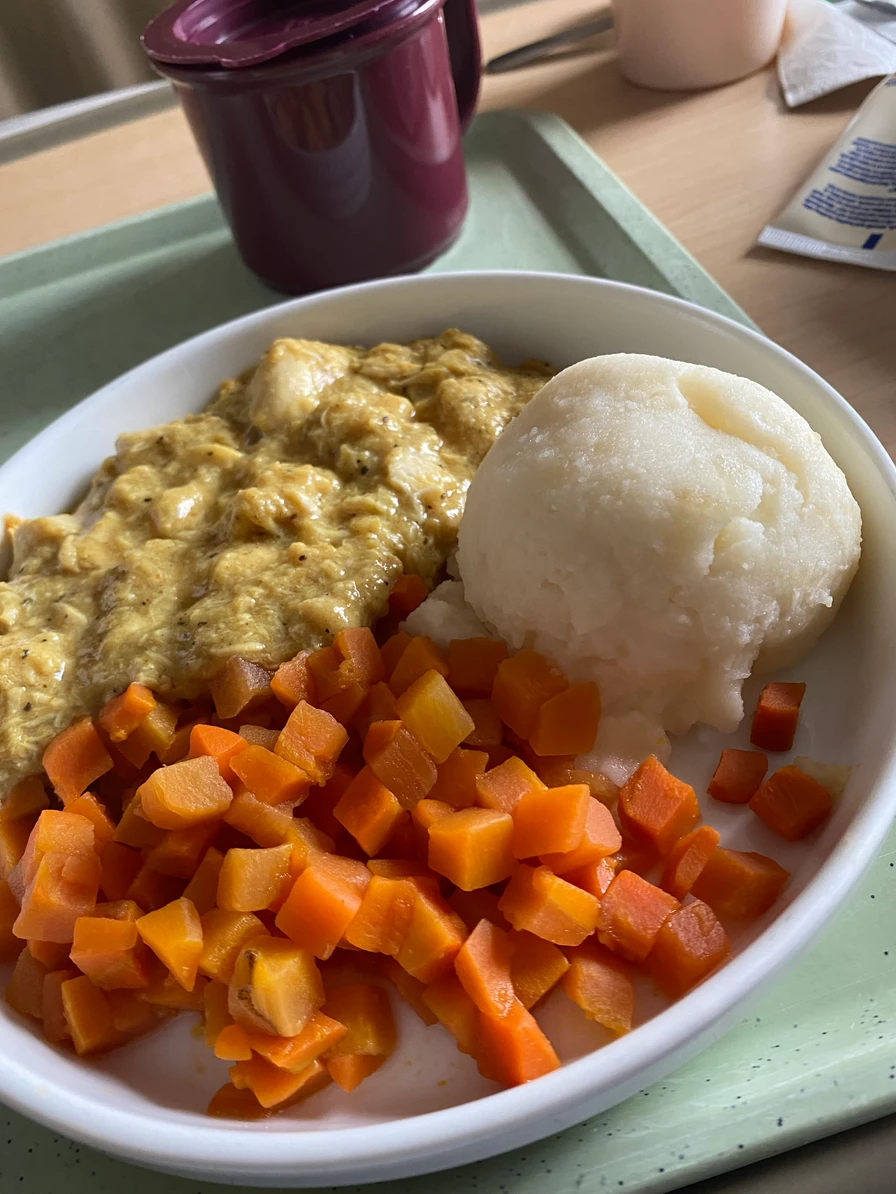
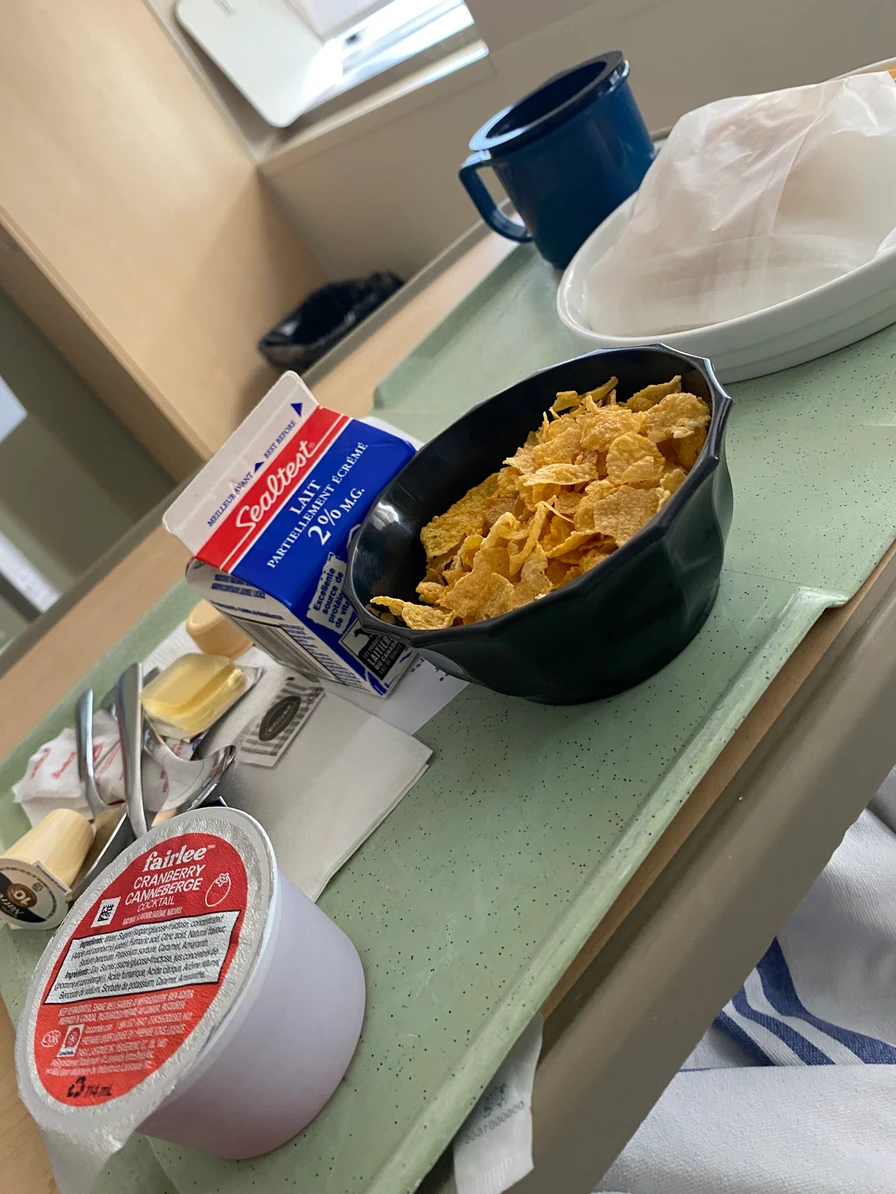
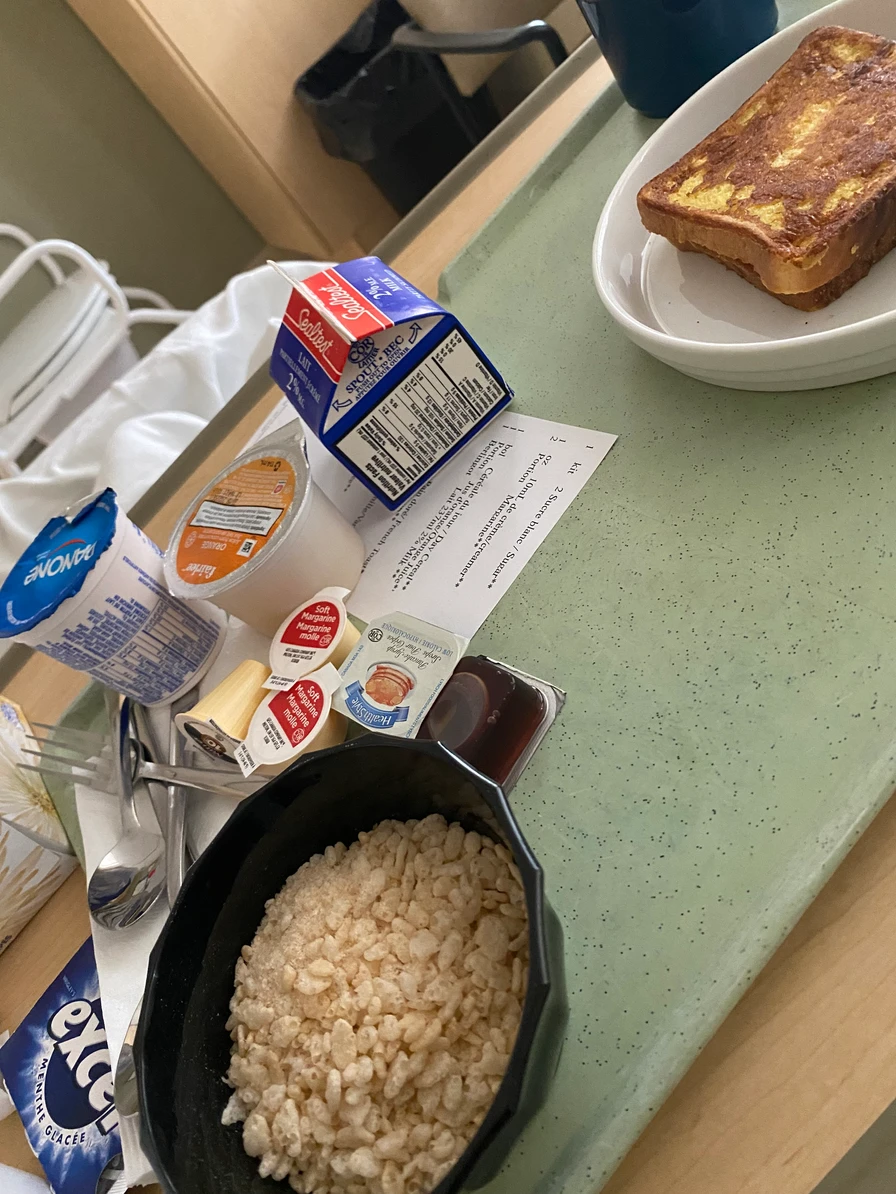

I was overall disappointed with the hospital food menu because they kept serving me hard foods or foods loaded with sugars & artificial flavours and very little protein. Sweetened yogurt, store-bought cupcakes & muffins, cereal and concentrated orange juice were recurring menu items. I even made a request for more soups and soft foods but it seems that went unnoticed.
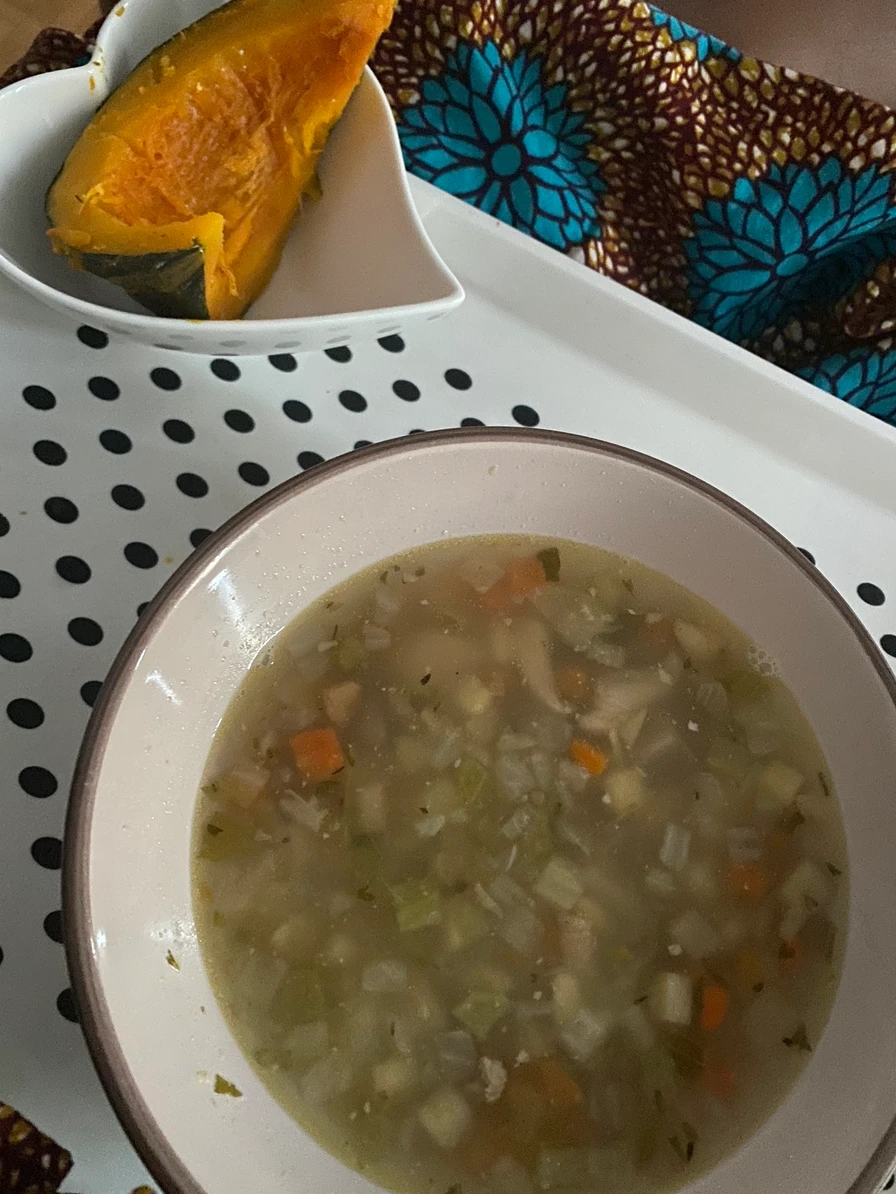
On day 2, my doctor informed me that my diet was not restricted and I could eat as normal but my body told me otherwise. It took me about a day to pass gas (very important) and pain meds make you very constipated. I stuck to soups and smoothies for the first 3 days and still needed a suppository to help assist with my first bowel movement, which occurred on Day 3.
I have since been on a laxative which I take twice a day to ensure I do not get constipated. Constipation leads to bad cramps and a hurtful stool which causes me to bleed. It’s extremely unpleasant and painful.
From Day 4, my appetite came back and my mom started introducing more mashed foods and harder foods liked mashed potatoes and beans, sliced mangoes and watermelons to my diet.
Since Day 7, I have been eating foods of all textures however, most of the foods seem to still be pretty soft – I’m talking rice, boiled plantains, roasted chicken, boiled fish, blended vegetable soups, eggs, sliced fruits and pan-fried vegetables.
You can see some examples of my meals below.





Since finding out that my scar is taking longer to heal, I’ve been incorporating more protein into my diet. This has been in the form of eggs, yogurt, milk, fish, chicken, beans and turkey.
I am also about to purchase some protein powder to add to my morning routine.
I try to limit my intake of red meat, salt, fried foods and processed foods (crackers, chocolate etc.) Spicy foods and citrus foods are also a no for me at the moment because pepper makes me cough (thus inducing abdominal pain) and acidic foods give me heartburn and nausea right now.
All the fried foods I have consumed have been home-made and the chocolate I nibble on occasionally is dark (at least 70% cocoa).
I know my body needs proper nourishment to help me recover internally and externally but I am also mindful that my physical activity has dropped drastically and I am probably burning less calories. Junk food is not a part of my diet as it also won’t provide any real nourishment needed for tissue repair.
Even at week 3, I still have not consumed a single pack of plantain chips (shocker!) and have not even craved it. With all these fresh fruits and veggies around me, I’m more interested in experimenting with different smoothie mixtures.
3) Physical activity: On my surgery day, the only movement I was able to manage post-myomectomy was to sit on the edge of my bed and this happened only because a kind nurse really insisted that I move my body even a little. The pain was insane. It’s incredible how many movements require your core muscles and I have learnt that the hard way.
An Intermittent Pneumatic Compression (IPC) device was strapped to my legs during my 4 days stay at the hospital as I could not walk. This was to prevent blood clots.
 From lying down to standing up to laughing to coughing to lifting your legs in bed, to lying on your side…your abdomen/core is involved. All of these movements were very painful the first 10 days post-surgery. This pain somewhat subsided from Day 12/13 but every time I over exert myself, I start to bleed vaginally.
From lying down to standing up to laughing to coughing to lifting your legs in bed, to lying on your side…your abdomen/core is involved. All of these movements were very painful the first 10 days post-surgery. This pain somewhat subsided from Day 12/13 but every time I over exert myself, I start to bleed vaginally. The vaginal bleeding has been on and off since my surgery date – but it is important to note that I had already been bleeding vaginally for 4 months prior to my myomectomy.
The vaginal bleeding has been on and off since my surgery date – but it is important to note that I had already been bleeding vaginally for 4 months prior to my myomectomy.
(Imagine! That woman in the bible who had been bleeding for years definitely had fibroids).
It is only from Day 4 that I began to actually take steps outside of going to sit on the commode to urinate or defecate. I had purchased a cane which has come in handy and which I still rely on (although less) at week 3. My mother had to hold my hand for the first 4 days or so of walking around my apartment and each time I needed to get off my couch (where I am still sleeping), I would need her assistance.
My mother had to hold my hand for the first 4 days or so of walking around my apartment and each time I needed to get off my couch (where I am still sleeping), I would need her assistance.
I have also been needing to go to the bathroom a lot more, especially at night. I don’t even consume a lot of water at night but I’m thinking it’s all of the fluids and IV’s being ejected from my body. I hope it stops by week 6! I can’t imagine still having to wake up 3+ times at night two months from now, yikes!
By Day 10, I was able to get 1,000 steps in one day! That was a milestone to me. I haven’t crossed the 2,000 step mark just yet because some days the pain is still worse and it feels like progress is not being made but I have to remind myself that this is my journey and I cannot compare my recovery to others’.
From Day 8, I was able to take my dry bath and dress myself without assistance, which is a huge milestone!
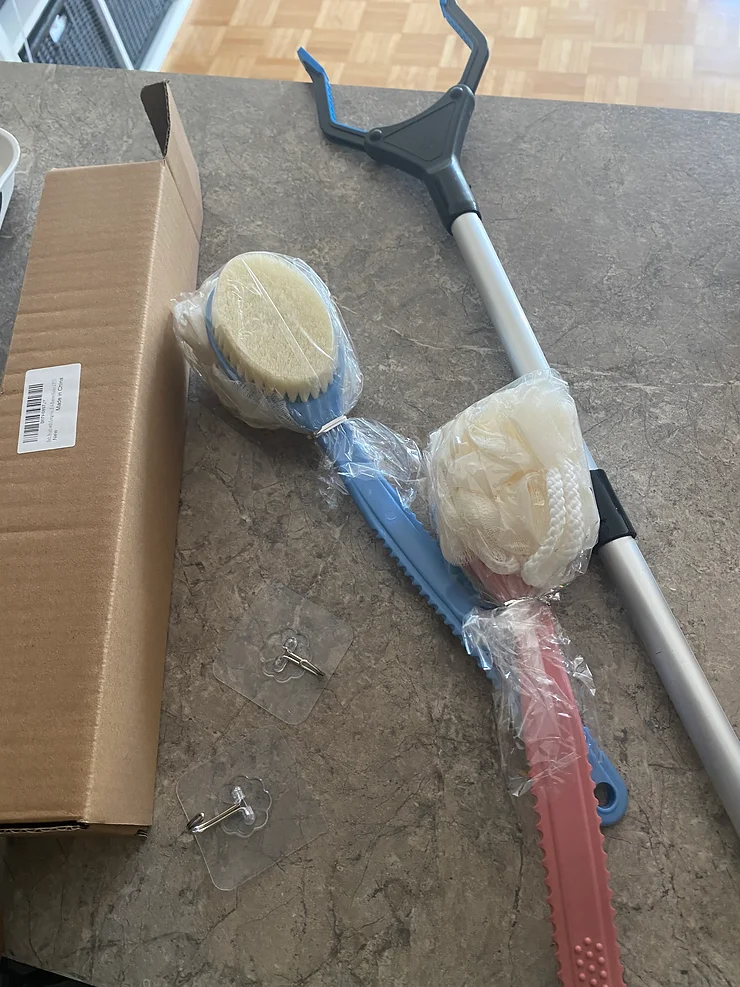
I still use my Reacher to pick up fallen objects and have a longer-reach back and foot scrub.
Whenever I feel a little better, I just want to do more and it’s hard to know my body’s limit until it manifests through pain or bleeding.
4) Pain levels: I have experienced debilitating menstrual cramps from fibroids (imagine sharp pelvic pain compounded with anal pain and then feeling like your uterus is about to drop out of your vagina all at once) and so I am no stranger to pain.
When I awoke from anaesthesia however, it was a different kind of pain I experienced. The first thing I said when I awoke was ‘pain’ and I heard someone tell a nurse to administer me morphine. My whole abdomen felt like a different part of my body. It hurt badly. A really sore type of hurt. Not a sharp pain. I could not even sit up.
I was receiving pain medication every 4 hours and a couple of times, I needed even more than that.
Morphine and I became good friends for the first 4 days post-surgery but ever since I was discharged, I have not had to take a single pill, although I have the prescription right here.
Day 2 was actually the most painful day for me because it’s when my catheter was taken out and I had to urinate on my own. I had lost temporary control of my bladder and could only feel excruciating pain, not realising I had to pee. I kept calling for a nurse to come but due to the extreme nursing staff shortage, no one was available.
As fate would have it, my mother arrived to visit me for the day right as I thought I would die from this pain. She told me it may be urine trying to come out and so asked me to sit up and helped to transfer me to a commode. Seconds later, what felt like burning urine rushed down my legs. It was so painful I began to cry but I felt so much relief afterwards.
The next 2 urinations were just as painful and I dreaded this process – also because I had to now get out of bed which in itself was a painful and tedious process.
From Days 5-11 or so, I was taking 2 Tylenol extra strength and 2 Advil extra strength twice a day to manage the pain. Nowadays, I’m at 1 tablet of each once a day or as is (if I start bleeding and cramping, I usually need to take 1 of each).
The most pain I feel is either when I’m getting up from lying down after more than 4 hours or if I’ve been wandering around the apartment for too long without sitting. I would rate this pain a 5 or 6.
It’s not nearly as bad as the pain and discomfort I felt on Day 5 when I experienced the worst and longest nausea I have ever had. It started around 5 pm and did not subside until 9 am the following morning. I could not eat a single thing and vomit was on the brink of my mouth the whole time.
My mom believes I consumed too many acidic food items that day and maybe ate too much food in general as well. I think I was over excited to get my appetite back.
As you can tell, there has been progress, even if it has been slower than I had anticipated given my overall good health prior to surgery.
I am learning to be patient with my body and enjoy this time of rest. I try not to worry about how my scar would look at the end of this but it’s hard sometimes when I have to look at it everyday while having my dry bath.
Any good movie or show recommendations are welcomed at this point although I don’t watch a lot of TV. I find myself sleeping more than any other activity!
Hopefully this post has been resourceful.
You may also want to check out my post on things I wish I had known before my myomectomy.
XOXO
Theankaraqueen
